Updated Frequently
Download the CDAnet Dental Office User Guide for use and training of dental office staff.
For a list of insurance carriers accepting CDAnet e-claims go to cda-adc.ca/carriers
Bilsland Griffith Benefit Administrators rebranding to Convyta Partners
November 18, 2025
As of October 1st, 2025, Bilsland Griffith Benefit Administrators (carrier ID 000128) rebranded to Convyta Partners. Please update the carrier name in your practice management system. Plan members ID cards will remain unchanged. The CDAnet claim processing configuration details will stay the same.
Telus AdjudiCare now accepts CDAnet file attachments
November 18, 2025
Telus AdjudiCare (carrier ID 000034) is now accepting CDAnet file attachments for claims and predeterminations submitted electronically.
Please update the carrier record in your practice management software to enable the attachment transaction:
- Attachment (09)
- Attachment Response (19)
The attachment option allows offices to send patient records such as x-rays, images or other documents along with the patient’s claim or predetermination. This claim feature reduces processing times as well as postage and administrative fees associated with the mailing of documents.
If you are unsure how to make the setting changes, please contact your software vendor.
Reminder to always verify patient’s eligibility with the CDCP Program
November 18, 2025
On October 17, Health Canada announced that the Canada Revenue Agency (CRA) corrected taxpayers’ adjusted family income calculations, which will affect eligibility and co-payment levels for some Canadian Dental Care Plan (CDCP) patients. Some patients will lose eligibility, while others will see changes to their co-payments.
Dentists are advised that no repayments will be required from patients or providers, and they should verify eligibility and co-payment details at each visit. Providers are encouraged to confirm whether patients have received updated coverage information and may contact Sun Life at 1-888-888-8110 for case-by-case reviews of mid-treatments involving crowns or dentures. Dental offices should direct patient inquiries to official CDCP communications or government sources.
Multi-Factor Authentication (MFA) coming soon to PSS website
October 15, 2025
As part of CDA’s ongoing commitment to information security, Multi-Factor Authentication (MFA) will soon be implemented on the PSS website to enhance security and help safeguard your data.
MFA adds an extra layer of protection by requiring users to verify their identity through more than one method, significantly reducing the risk of unauthorized access.
All users are reminded not to share accounts; each user should have their own account if they require access to the PSS website. Sharing accounts can lead to serious security risks; it creates challenges for auditing who made changes, it increases the chance of unauthorized access, and it weakens accountability. Sharing accounts can also result in account breaches if credentials are mishandled.
Creating individual accounts ensures personalized permissions, and a safer, more reliable system. Please review your office’s current access and ensure all users have individual accounts before MFA is activated.
Canada Life introduces updates to EOB responses
October 15, 2025
Starting October 17, 2025, Canada Life (Carrier ID 000011) will introduce updates to enhance real-time Predetermination (03) Explanation of Benefits (EOB) responses, especially when Canada Life is both the primary and secondary payor.
Offices with Canada Life set to use CDAnet version 4 in their software, who submit a predetermination under the primary plan with secondary plan details will now receive a real-time EOB (instead of just an acknowledgment) when services can be assessed immediately. Providers can still submit separate secondary plan predetermination requests for full coverage confirmation.
Please contact your software company if you require assistance updating your practice management software.
Read the full communication here.
Quikcard changing network providers
June 27, 2025
Effective June 27, 2025, Quikcard (carrier ID 000103) will transition from the instream network to the TELUS network. Please ensure to update the Quikcard carrier record in your practice management system (PMS) to avoid claims being rejected.
If you require assistance updating the carrier details, please contact your PMS vendor.
Johnson Insurance rebranding to belairdirect
June 27, 2025
Effective July 1st, 2025, Johnson Insurance (carrier ID 627265) will be rebranding to belairdirect. Please update the carrier name in your practice management system. Plan members will be issued a new benefit card and note that the carrier ID 627265 will remain the same, only the name requires change.
Also, the CDA carrier record on our website has been updated to include regional mailing addresses for submitting standard dental claims when necessary.
Read the full notice here.
CDCP update
June 27, 2025
Health Canada has made an interim update to the Preauthorization Checklist for Crowns. The Periodontal Screening Record (PSR) is now accepted when a full periodontal chart isn’t available. This change hasn't yet been reflected in the Dental Benefits Guide. If providers contact Sun Life, they might still be referred to the existing documentation listed in the Guide, but section 5.1 outlines what to do when only partial documentation is submitted. You can find the updated version in the Oral Health Provider Toolkit.
Additionally, Health Canada clarified timelines for denture insertions under CDCP to prevent financial hardship:
- Provisional/transitional dentures must be inserted within 7 days of extractions.
- Immediate dentures must be placed within 45 days of extractions.
- After those timeframes, other kinds of dentures would need to be requested.
- Permanent dentures can only be inserted at least 6 months after provisional/transitional ones.
Read the full notice here.
Enhanced file security with Secure Send API
June 23, 2025
The CDA has updated the CDA Secure Send service to strengthen security by restricting file uploads of potentially harmful file extensions. Specific files extensions will automatically be excluded from messages and clearly marked as removed in the final Secure Send message report PDF, attached to each message that’s sent or received. No action is required from users, as the process is handled entirely within the system.
To see a complete list of the restricted file extensions, click here
Canada Post workers could strike again soon
May 15, 2025
Last year’s Canada Post strike caused considerable disruption to Canadian businesses and consumers. Many dental offices that rely on mail delivery found themselves waiting an extended period of time to receive cheques from claims processors.
The strike ended with an extension on the existing agreement until May 22, 2025. While the Canadian Union of Postal Workers (CUPW) and Canada Post are currently continuing negotiations to avoid another strike, the May 22 date is quickly approaching.
To avoid potential delays, dental practices should consider using direct deposit with the insurance carriers. This will ensure that payments are received promptly, even in the event of a strike.
Keep up with the latest updates on negotiations:
Help us improve CDAnet claim processing!
May 15, 2025
The Canadian Dental Association is committed to continuously improving our services to better support dental practices like yours. We understand that an efficient claims process is vital for your operations, and we would greatly appreciate your insights to help us improve claims processes for all dental practices across Canada.
If you are someone who submits claims and you would like to make a difference, please provide us with your contact information by completing the details in this link.
How to Share Your Insights
You do not need to be an expert and there is plenty of flexibility to allow you to participate when it suits you. Your involvement may include responding to short surveys, or you might be invited join a focus group. We may reach out to you approximately 1-4 times a year to gather your input on key aspects of the claims process, our website or CDA Secure Send service. Participation is optional and you can request not to be contacted if you change your mind.
Thank you in advance for your time and valuable time and input. Together, we can improve claims processes for all dental practices across Canada.
Coughlin & Associates and Funds Administrative Service Inc. (FAS) have switched to TELUS Adjudicare
May 15, 2025
Coughlin & Associates (carrier ID 610105) and Funds Administrative Service Inc. (FAS) (carrier ID 610614) have started processing member claims with TELUS AdjudiCare (carrier ID 000034). They have been removed them from the list of active CDAnet carriers. By now, plan members would have received new benefit cards with new group and certificate numbers.
Please ensure you verify the patient’s benefit card to identify if the carrier information should be updated in your practice management software for CDAnet e-claims.
TELUS AdjudiCare is a claims processor that provides claim processing services for many third-party administrators (TPA’s), using the carrier ID 000034.
If you have any questions, you can contact TELUS Health at 1-866-272-2204.
CDCP Audits & Clawbacks
May 15, 2025
CDA and the Provincial and Territorial Dental Associations (PTDAs) are aware of increased audits and clawbacks under the Canadian Dental Care Plan (CDCP), mainly for claims during the early implementation (May–June 2024) due to unclear guidance.
Common issues triggering audits and clawbacks include the following, but are not limited to:
- Using one dentist’s Unique Identifier Number (UIN) on claims for all dentists from the clinic. This goes against the terms of the CDA subscriber agreement and should never be followed.
- Insufficient documentation to justify treatment.
- Fluoride treatments deemed unnecessary.
- Missing “complete” in treatment records (e.g., for scaling).
- Dentists are encouraged to carefully review your documentation and the CDCP Dental Benefits Guide.
Questions? Please contact your Provincial/Territorial Dental Association for more information.
GMS Insurance Inc, Group Medical Services & Groupe Premier Medical Accept Coordination of Benefits (COB) CDAnet 07 Transaction
March 28, 2025
Effective March 28th 2025, GMS Insurance Inc (carrier ID: 610218), Group Medical Services (carrier ID: 610217) and Groupe Premier Medical (carrier ID: 610266) will start accepting COB claims through CDAnet!
Whether GMS Insurance Inc, Groupe Medical Services or Groupe Premier Medical are the primary and secondary or just the secondary carrier, you can send a COB 07 claim. The benefits for the secondary claim will be processed based on the returned Explanation of Benefits (EOB) from the primary claim. There is no need to submit a paper claim form.
To make this option available in your practice management software, please update the carrier records to include the COB option. Please contact your software company if you require assistance updating your practice management software.
CDCP Updates on Preauthorization
March 28, 2025
Sun Life would like to remind all offices that they are currently experiencing a high volume of preauthorization submissions, resulting in varied turnaround times. To help minimize further delays, please ensure that preauthorizations are submitted only submitted once.
Preauthorization requests are being processed on a first-come, first-processed basis and decisions will be available once your submission is processed.
Above frequency limit preauthorization request
Health Canada and Sun Life are aware that preauthorization submissions through CDAnet for codes exceeding frequency limits are being declined. They are currently working to resolve this problem. In the meantime, dentists should submit these requests by mail.
CDCP Coverage Renewals
March 28, 2025
The Government of Canada has started its annual reassessment of individuals covered under the Canadian Dental Care Plan (CDCP) to confirm that they continue to meet all eligibility requirements.
CDCP patients (or delegate) must complete the renewal process prior to June 1, 2025. Reminding any current patients covered under the plan to renew, may avoid a gap in their coverage. Patients will receive a letter from the Government of Canada informing them that they must renew, with instructions on how.
Patients who are no longer eligible for the CDCP or do not renew will have their CDCP coverage end on June 30, 2025. Please remember to always verify the patient’s eligibility with the CDCP program!
CDCP Policy Information – Check for accuracy!
March 07, 2025
The Canadian Dental Care Program's policy number is 333333 (which consists of 6 digits). It's important to pay attention to this to avoid errors, such as mistakenly entering a policy number with 5 or 7 digits.
Starting March 9th, if a predetermination or claim is submitted to Sun Life with a policy number that has more than 6 digits or a member ID that exceeds 11 characters, the submission will be rejected, and an error message will be sent back. In such cases, please update the patient's records and resubmit the transaction to Sun Life.
Update on CDCP Dental Benefits Guide and Preauthorization requests
March 07, 2025
Health Canada has updated the Canadian Dental Care Plan (CDCP) Dental Benefits Guide, with changes marked “updated” in the related sections. These updates aim to clarify preauthorization and documentation requirements. You can access the latest version of the guide below.
Additionally, Health Canada has advised that Sun Life is managing a high volume of CDCP preauthorization requests, which are processed in the order received. To avoid unnecessary delays, dentists are encouraged to not submit the same submission or claim multiple times. Members are encouraged to review the updated guide and follow the recommended submission process to help streamline approvals.
CDCP Dental Benefits GuideSaskatchewan Blue Cross Updated Supported Transactions
March 07, 2025
Just a reminder that as of March 4th, 2025, Saskatchewan Blue Cross (carrier ID 000096) is now supporting many new CDAnet Transactions. Please ensure your software is updated with the following transactions:
- COB Claim (07)
- If the primary insurer is different than SBC, send the COB claim using the COB 07.
- If SBC is the primary and secondary insurer, send the claim or predetermination, SBC will automatically coordinate the benefits and return two EOB’s.
- Claim EOB (21)
- Claim Reversal (02)
- Claim Reversal Response (12)
- Predetermination (03)
- Predetermination Acknowledgement (13)
- Predetermination EOB (23)
- Request for Outstanding transaction (04)
- Outstanding Transaction Response (14)
- Age limit – 90 days
Also, the following policy information has been updated:
- Policy Numbers: 5 digits (numeric)
- Division Numbers: N/A
- Certificate Numbers: 1-10 digits (alpha-numeric)
To ensure these transactions are available in your software for Saskatchewan Blue Cross, you will need to update the settings in your practice management software. If you are unsure how to make these changes, please contact your software vendor for assistance.
For a complete list of transactions supported by Saskatchewan Blue Cross, please visit the CDAnet Carrier page.
SFMM has changed claims processor from Express Scripts Canada to GreenShield Insurance
February 26, 2025
On January 1, 2025, Syndicate des fonctionnaires municipaux de Montréal (SFMM) began using GreenShield Insurance (carrier ID 000102) to process their CDAnet electronic claims.
SFMM plan members must provide their new plan member information. Their member card includes an 8-digit number and a 2-digit suffix identification number (see below example). For dental coverage, only the first 8 digits are required; please disregard the dash and 2-digit suffix.

|
GreenShield will only accept CDAnet electronic claims for services rendered on or after January 1, 2025. Claims for services prior to this date must be submitted using the manual claim form and sent directly to SFMM by March 1, 2025.
Syndicat des fonctionnaires municipaux de Montréal (SFMM)
8790, avenue du Parc
Montréal (Québec)
H2N 1Y6
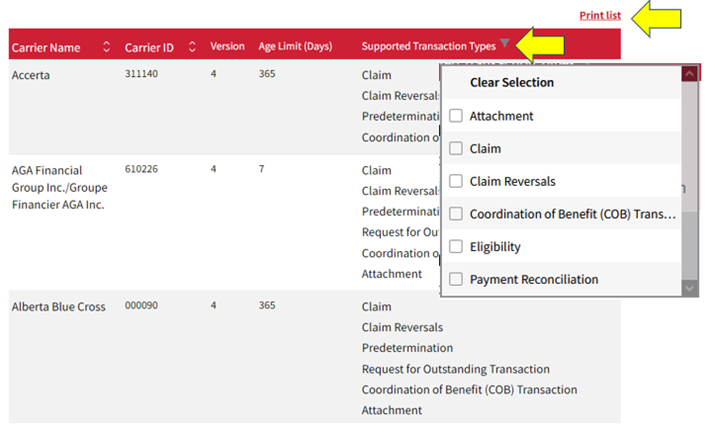
New features available on the CDA Carrier List Page
February 26, 2025
You can now print and sort carriers by the “Supported Transaction Types”! These enhancements are designed to improve your user experience and easily find carriers that support the specific transaction types you need, saving you time and effort.
Try it out! Simply go to the CDAnet Carriers List page, click the “filter” icon next to the “Supported Transaction Types” label, and select one or more transaction types. The list will automatically update to display carriers that match your criteria. Also just above, is the “Print List“ option.
|
Ensure accurate carrier information on your patient's Explanation of Benefits
February 26, 2025
Including accurate carrier information on your patient's Explanation of Benefits (EOB) claim responses is important. The patient claim documents must correctly reflect the insurer, program name, and benefit plan information. For example, the office software should no longer have Canada Life listed as Great West Life or NIHB listed as First Canadian Health.
Ensuring carrier information is updated in your software can help prevent errors and ensure all claim information and patient EOB documents are accurate. If you require assistance, please contact your software vendor.
For a complete list of carriers, please visit the CDAnet Carrier Listing on our webpage.
Dental Benefits Education Materials for Patients and Dentists
February 26, 2025
The Canadian Dental Association (CDA) is pleased to announce the launch of new Dental Benefits Education materials, designed to help patients better understand dental benefits while also supporting dentists' understanding and discussions with patients.
Helpful resources like downloadable PDF guides, videos, and provincial/territorial public program information are available on our webpage.
Visit Understanding your Dental Benefits on CDA’s website.
Saskatchewan Blue Cross Updated Supported Transactions
February 26, 2025
Effective March 4th, 2025, Saskatchewan Blue Cross (carrier ID 000096) will start accepting the following additional CDAnet transactions:
- COB Claim (07)
- If the primary insurer is different than SBC, send the COB claim using the COB 07.
- If SBC is the primary and secondary insurer, send the claim or predetermination, SBC will automatically coordinate the benefits and return two EOB’s.
- Claim EOB (21)
- Claim Reversal (02)
- Claim Response (12)
- Predetermination (03)
- Predetermination Acknowledgement (13)
- Predetermination EOB (23)
- Request for Outstanding transaction (04)
- Outstanding Transaction Response (14)
Also, the following policy information has been updated:
- Policy Numbers: 5 digits (numeric)
- Division Numbers: N/A
- Certificate Numbers: 1-10 digits (alpha-numeric)
- Age limit – 90 days
To ensure these transactions are available in your software for Saskatchewan Blue Cross, you will need to update the settings in your practice management software. If you are unsure how to make these changes, please contact your software vendor for assistance.
For a complete list of transactions supported by Saskatchewan Blue Cross, please visit the CDAnet Carrier page.
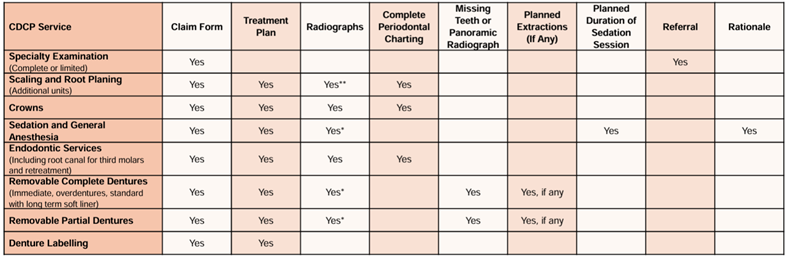
Important Update on CDCP Preauthorizations and Attachments
December 20, 2024
CDA continues to communicate with Health Canada and Sun Life regarding the Canadian Dental Care Plan (CDCP) challenges related to sending predetermination, attachment and claim messages. Note that what the CDCP calls a “preauthorization” is sent with your software’s “predetermination” function.
During this adjustment period, please note the following points to help clarify processes and timeline expectations.
- Sun Life is currently experiencing very high volumes of CDCP claims and is working to reduce its processing times. Please allow a minimum of 2 weeks before calling to inquire about the results of a claim or preauthorization.
- Preauthorizations and claims do not appear in the Sun Life Direct portal until they have been processed by a Sun Life agent. Therefore, the status of a submitted preauthorization and attachment cannot be viewed on the Sun Life Direct portal while it's pending to be processed. When the preauthorization is processed, an Explanation of Benefits (EOB) will be available on the Sun Life Direct portal.
- Attachment messages to support preauthorizations should be submitted on the same day, to ensure that supporting documents are included when Sun Life processes a preauthorization.
- Ensure that the required documentation is submitted with a preauthorization. A quick reference chart is available on the Sun Life Direct portal.
|
- Please refer to Sun Life’s CDCP information document for complete details on claim processing: Canadian Dental Care Plan (CDCP) - Useful information to help you navigate claims processing under the Canadian Dental Care Plan.
- More software vendors are starting to implement the attachment feature. It's possible that your software provider has added this feature to its newer versions. Check the CDAnet Certified Vendor list to confirm if your software vendor has the attachment functionality. Alternatively, you can use the Standard Dental Claim form to submit a CDCP preauthorization request, along with the required documentation.
- Please ensure that patient notes or other supporting documents for a predetermination are included and sent with the attachment message. The predetermination message does not contain this information. To confirm the correct process for sending these documents in the attachment message, please consult your software vendor.
Green Shield Canada becomes GreenShield Insurance
December 20, 2024
Effective January 1st, 2025, Green Shield Canada will become GreenShield Insurance. Their CDAnet carrier ID 000102 will remain the same; however, you will need to update their carrier name in your dental office software on or after January 1st.
Green Shield Canada full communication
Reminder: Johnston Group Accepts Coordination of Benefits (COB) CDAnet 07 Transaction
December 20, 2024
Johnston Group is now accepting COB claims through CDAnet! Whether they are the primary or secondary plan carrier, you can send your patient's COB claims electronically.
To have this option available in your practice management software, please ensure that you update their carrier record with the COB option.
- CDAnet version – must be version 4
- Coordination of Benefits (COB) Claim (07)
Whether Johnston Group is the primary and secondary or just the secondary carrier, you can send a COB 07 claim. The benefits for the secondary claim will be processed based on the returned Explanation of Benefits (EOB) from the primary claim. There is no need to submit a paper claim form.
Please contact your software company, if you require assistance updating your practice management software.
Johnston Group Accepts Coordination of Benefits (COB) CDAnet 07 Transaction
October 31, 2024
Johnston Group is now accepting COB claims through CDAnet! Whether they are the primary or secondary plan carrier, you can send your patient's COB claims electronically.
To have this option available in your practice management software, please ensure that you update their carrier record with the COB option.
- CDAnet version – must be version 4
- Coordination of Benefits (COB) Claim (07)
Whether Johnston Group is the primary and secondary or just the secondary carrier, you can send a COB 07 claim. The benefits for the secondary claim will be processed based on the returned Explanation of Benefits (EOB) from the primary claim. There is no need to submit a paper claim form.
Please contact your software company, if you require assistance updating your practice management software.
Update on the adjudication service for AGA Financial Group Inc. n
October 31, 2024
Starting in November 2024, AGA Financial Group Inc. will issue new benefit cards that include a new ID number. Please ensure you ask your patients for their updated information, as claims submitted with the previous ID number will be rejected.
Read the full communication here.
Canada Life is now available on providerConnect
October 31, 2024
Dentists and staff can now find the following Canada Life information on providerConnect.
- Dental predetermination status
- Patient claim history and status when it’s payable to a dentist
- Your statement, which you currently get by secure email
- Claim payment schedules to find out when you’ll get paid
Find out more at welcome.canadalife.com/dental-provider.
The Benefits Trust - address update
October 31, 2024
Benefits Trust (The) has notified us of a change in their address. Please ensure that the manual claim forms in your software is updated with the following mailing address.
Benefits Trust (The)
1453 Pelham St, P.O. Box 41
Fonthill, ON L0S 1Eo
CDAnet Attachment Feature – A better way to send patient documentation!
October 22, 2024
Predeterminations can require x-rays and other documentation and often, these can be sent electronically with CDAnet if your software supports the “Attachment” feature.
Starting November 1, 2024, the Canadian Dental Care Plan (CDCP) will be accepting preauthorization requests for Schedule B services, and these will require a predetermination and patient documentation, which Sun Life will accept electronically.
How does it work?
Each company’s software may have different processes, but the basic steps are the same. First, you send a predetermination, then you send the attachment. You can include up to 30 files in one attachment message with a total combined file size of 7 MG. Since the attachment message has the predetermination message ID, the insurance company can easily link the predetermination and attachments so the request can be reviewed quickly.
The method used to communicate the predetermination result varies by claim processor. It may be available in a “provider portal,” sent by mail, or returned with a CDAnet Request for Outstanding transaction message. Either way, using the CDAnet Attachment feature will be much faster than mailing the claim form and documentation.
How do I know if I can send an attachment?
You can check the CDA Certified Vendor List to determine if the software you use supports the Attachment feature. If your software doesn’t support attachments, ask your vendor if they plan to support it. We know that many vendors have plans to support it, and some are working on it right now.
Also, if your practice management software offers the attachment feature but you are unsure how to use it, we suggest checking the help centre for manuals or training videos. You can also contact your software company to ask for information.
Will it save time and money?
With the CDAnet Attachment, there is no need to print documents like quality x-rays, claim forms, or mailing envelopes. This traditional method is more time consuming, costly and leads to longer wait times for obtaining the patient’s preauthorization approval and scheduling appointments.
The CDAnet Attachment provides an automatic acknowledgment response, that confirms the documentation was received. Coverage results are faster without the mail time, and you can schedule patients for treatment sooner.
More carriers support the CDAnet Attachment. You can count on sending patient documentation to these carriers electronically. Try the CDAnet Attachment feature in your software.
Carriers accepting CDAnet Attachment
- Alberta Blue Cross
- Beneva/La Capitale
- Canada Life
- Desjardins Insurance
- TELUS AdjudiCare
- AGA Financial Group Inc. /Groupe Financier AGA Inc.
- Quikcard
- Sun Life Financial
Medavie Blue Cross and Saskatchewan Blue Cross changing network providers
September 26, 2024
As of September 26, 2024, both Medavie Blue Cross (carrier ID 610047) and Saskatchewan Blue Cross (carrier ID 000096) will be changing from the Telus Network to the Instream Network.
If you experience any issues transmitting, please contact your PMS vendor.
The PBAS Group accepts CDAnet e-claims for additional plans
September 26, 2024
Effective September 1, 2024, The PBAS Group (carrier ID 610256) will be accepting Plan 012 – UCGSA Benefit Plan and Plan 013 – UCGSA Staff Benefit Plan.
Starting October 1, 2024 they will be accepting Plan 830 – Millwrights’ Health and Welfare Trust Fund of Alberta.
When sending CDAnet e-claims for patients with these plans, ensure your practice management software is set with the following carrier information:
The PBAS Group
Carrier Code: 610256
Version: 4
Read the full notice and view a list of plans currently accepting CDAnet e-claims.
Sun Life CDCP Claim rejections – name mismatch
August 8, 2024
When submitting a patient’s claim to Sun Life under the CDCP program, ensure that the patient’s name matches the name on the CDCP card. If the names don’t match, Sun Life will reject the claim, and return an acknowledgment with the error message “Some information is incorrect/missing. Please correct and resubmit”.
If you are still experiencing issues, you can check the status of the claim by signing into the CDA’s practice support services website for your office and clicking the ITRANS Claims tab. Additionally, you can use the chat tool to connect to the CDA Help Desk for assistance.
Accerta now accepts Coordination of Benefits - 07
August 8, 2024
Accerta is now accepting coordination of benefit (COB) claims with CDAnet! They will accept a COB-07 claim when they are both the primary and secondary carrier or just the secondary carrier (e.g., for CDCP claims).
To send Accerta a COB–07 claim, you will need to update the Accerta carrier record in your practice management software (PMS).
Accerta carrier ID. 311140 must be set to the following:
- CDAnet version – must be set to version 4
- Coordination of Benefits COB claim (07) – enabled
View Accerta’s full claim details on our CDAnet Carrier webpage
Please note: a COB claim can only be sent if the primary carrier returned an EOB, and the EOB is version 4. All carriers should be set to CDAnet version 4 in your PMS, as version 2 is retired. If you encounter an error with your COB claim, check the primary carrier version in your PMS. If it requires updating to version 4, make the change. The next COB claim to Accerta that includes the same primary carrier will be processed.
Please contact your software company if you need assistance updating your PMS or sending a COB claim.
Know Before You Go - Canadian Dental Care Plan (CDCP) Resources
August 8, 2024
The CDA offers useful resources, FAQs, and links to program information for dentists, staff, and the public to access about the Canadian Dental Care Plan (CDCP).
In late May, CDA launched a national public awareness campaign aimed at dispelling common misconceptions about the CDCP. These misconceptions include:
- For many patients, treatment under the CDCP will not be free.
- Not all providers are participating in the CDCP.
- Additional care is not available until November.
As part of the campaign, a printable appointment reminder resource was made available for download on the CDA website. Visit the page regularly for new information.
Johnston Group Accepts Coordination of Benefits (COB) CDAnet 07 Transaction
July 2, 2024
Johnston Group is now accepting COB claims with CDAnet! Whether they are the secondary plan carrier or not, you can send your patient's COB claims electronically.
Please ensure that you update their carrier record with the COB option in your practice management system.
View Johnston Group (627223) full claim details
- CDAnet version – must be version 4
- Coordination of Benefits (COB) Claim (07) - enabled
Johnston Group COB options:
If Johnston is the secondary carrier – When the primary carrier is CDAnet version 4, send the secondary benefit claim using COB 07 transaction. The secondary claim benefits will be adjudicated based on the returned EOB from the primary claim.
If Johnston is primary and secondary - Send the primary claim to Johnston, and if an EOB is returned, send the secondary claim using the COB 07 transaction. The secondary claim benefits will be adjudicated. There is no need to submit a paper claim form.
Please contact your software company, if you need help updating your practice management software or help sending a COB claim.
Alberta Health Dental Benefits has switched to Alberta Blue Cross Carrier ID 000090
The administration of the Alberta Health Dental Benefits including Dental Assistance for Seniors Program (DASP) and Low Income Health Benefit (LIHB) program dental benefits has transitioned from the ADSC carrier ID 000105 to Alberta Blue Cross carrier ID 000090.
Alberta Blue Cross does not support the eligibility transaction, however, a Predetermination can be submitted to receive information on a patient's coverage.
What's required?
Dental offices must update the patient records in the practice management system to ensure claims are sent to Alberta Blue Cross, carrier ID. 000090.
Read the full communication here
Sun Life age limit now 365 days
Effective immediately the age limit for all claims sent to Sun Life Carrier ID 000016 is 365 days. The age limit was recently changed from 7 days to 30 days, now 365 days. Please update their “age limit” setting in your practice management software to ensure claims over 30 days can be submitted to Sun Life.
Industrial Alliance now supports claim reversals
You can now submit a claim reversal to Industrial Alliance Carrier ID 000060. Please update your practice management software to enable the transaction:
- Claim Reversal (02)
- Claim Reversal Response (12)
Humania now processing with Green Shield
Humania no longer processes claims using carrier ID 000080 (previously processed by Express Scripts). Instead, all claims should now be submitted to Green Shield, carrier ID 000102. Please ensure that your patient records are updated with this new information.
Alberta Health Dental Benefits is switching to Alberta Blue Cross Carrier ID 000090
June 3, 2024
Effective June 3, 2024, the administration of the Alberta Health Dental Benefits including Dental Assistance for Seniors Program (DASP) and Low Income Health Benefit (LIHB) program dental benefits will transition from the ADSC carrier ID 000105 to Alberta Blue Cross carrier ID 000090.
What's required?
Dental offices must update the patient records in the practice management system to ensure claims are sent to Alberta Blue Cross, carrier ID. 000090.
- Until June 3, 2024, all inquiries about coverage, claims, exception requests, and payment should continue to be directed to the ADSC at 1-800-232-1997.
- Any questions related to the transition of claims administration can be directed to Alberta Blue Cross.
- As of June 3, please direct all DASP and LIHB program inquiries to Alberta Blue Cross.
This change does not impact eligibility; however, there will be upcoming changes to coverage, including the exceptions submission process.
Read the full communication here
Sun Life is now accepting CDAnet Attachments
May 13, 2024
You can now securely submit patient information to Sun Life using CDAnet. If your practice management software allows attachments, you can send patient charts and/or x-rays along to support claims and predeterminations all within your practice management software (PMS). To know if your software supports the CDAnet Attachment, check the CDAnet Certified Vendors list.
To enable CDAnet attachments for Sun Life, check the Sun Life settings in your PMS. If you need assistance with this, please contact your software vendor.
Sun Life will advise offices when to send x-rays and documents to support a claim or predetermination.
Sun Life joins the following carriers that accept the CDAnet Attachment:
- AGA Financial Group
- Alberta Blue Cross
- Beneva/La Capitale
- Canadian Life
- Desjardins Insurance
- Quikcard
- Sun Life
- UV Insurance
- Manulife expected 2025
Read more about Sun Life’s support of the CDAnet attachment.
Sun Life Carrier ID 000016 Age Limit Change
Sun Life’s Age limit has increased from 7 days to 30 days. Please be sure to update Sun Life’s carrier settings in your PMS.
Canadian Dental Care Plan (CDCP) Resources
Health Canada and Sun Life have CDCP resources available on Sun Life’s website including but not limited to:
- CDCP claim submission information
- Claims submitted for the CDCP plan will be identified by plan number 3333333.
- Paper claims will only be accepted in November 2024.
- Services requiring preauthorization won’t be covered until November 2024.
- Coordination of benefits
- Defining the primary payor
- Provincial and territorial social dental programs.
- Other federal social dental programs.
For more information, please visit Sun Life’s website at https://www.sunlife.ca/sl/cdcp/en/provider/
Did You Know?
You can access CDAnet claims, predetermination, and attachments sent from your office, and view the responses from the claims processor in PSS? All you need to do is sign into PSS and click on the ITRANS Claims tab. You can choose to view all office transactions or by dentist. This feature can be very helpful in troubleshooting any issues with claims.
Canada Life will no longer accept dental claims submitted with Public Service Health Care Plan (PSHCP) plan numbers
March 18, 2024
Effective March 19, 2024, Canada Life the administrator of Public Service Dental Care Plan (PSDCP) will no longer accept dental claims submitted with Public Service Health Care Plan (PSHCP) plan numbers 52111, 52112, 52113, 52114, and 52115. Instead, dental offices can expect to receive an Acknowledgment response with the error message:
Incorrect plan#. Confirm plan & ID and resubmit to correct carrier.
If you receive this response, please ask the patient to provide you with the correct plan and certificate number. Update your records and resubmit the claim to Canada Life.
The Public Service Dental Care Plan (PSDCP) and the Public Service Health Care Plan (PSHCP) are both administered by Canada Life. These plans have unique plan and certificate ID numbers, however, Canada Life continues to receive dental benefit claims from dental offices with the PSHCP plan numbers causing delays with claim adjudication and the communication of benefit reimbursement. To ensure proper claim submission, Canada Life will provide an Acknowledgement response with the referenced error message.
For more information, including FAQ’s please read Canada Life’s communication.
Industrial Alliance has upgraded its dental claim system to CDAnet v4
January 31, 2024
Industrial Alliance, (carrier ID 00060) and Industrial Alliance Pacific Life Insurance Co. (carrier ID 00024) have upgraded to CDAnet version 4. The upgrade requires dental offices to update both carrier records in the office practice management software. Also included are some carrier claim detail changes.
Effective January 31st - Industrial Alliance Pacific Life Insurance Co. Carrier ID 000024
CDAnet version – change from 2 to 4
Multipart Predeterminations – change to Y (supported)
Request for Outstanding Transaction (04) – change from Y (supported) to N (not supported)
Outstanding Transaction Response (14) – change from Y (supported) to N (not supported)
Claims Processor help desk - 1-877-422-6487
Effective January 31st Industrial Alliance Carrier ID 000060
CDAnet version – change from 2 to 4
Multipart Predeterminations – change to Y (supported)
Request for Outstanding Transaction (04) – change from Y (supported) to N (not supported)
Outstanding Transaction Response (14) – change from Y (supported) to N (not supported)
Claims Processor help desk - 1-877-422-6487
Manulife Financial, Affinity Markets will be processing CDAnet version 4 claims.
January 31, 2024
Effective January 31, 2024, Manulife Financial, Affinity Markets will be processing CDAnet version 4 claims! All offices must update their practice management software to change their carrier ID. 311113 CDAnet version setting from 2 to 4.
If you require assistance updating the carrier details, please contact your practice management software vendor.
The Benefits Trust will be processing CDAnet version 4 claims.
January 31, 2024
Effective January 31, 2024, Benefits Trust will be processing CDAnet version 4 claims! All offices must update their practice management software to change the Benefits Trust (carrier ID 610146) CDAnet version from 2 to 4.
The Benefits Trust is also working on moving from batch processing mode to real-time. We will communicate more on this when it is available.
If you require assistance updating the carrier details, please contact your practice management software vendor.
Manulife Financial has upgraded its dental claim system to CDAnet v4
January 22, 2024
Effective January 22, 2024, Manulife will be processing claims using CDAnet version 4! All offices must update their practice management software to change the Manulife (carrier ID 610059) CDAnet version from 2 to 4.
A key benefit to their upgrade is the v4 explanation of benefit response will now allow offices to send more coordination of benefits claims with CDAnet.
When Manulife is the primary carrier, now you can send a coordination of benefits claim (COB 07) to carriers who support the COB 07 transaction (see the list here). Their carrier record must be set to version 4 in your software for this to be available.
Manulife is working on supporting the COB 07 and Attachment transactions, although these will still take some time before being ready for you. We will let you know when these transactions are available.
If you require assistance updating the carrier details, please contact your practice management software vendor. For all other inquiries, please contact CDA’s helpdesk at 1-866-788-1212
National Life of Canada is moving to CDAnet v4
January 19, 2024
National Life of Canada (carrier ID 000021) claim processing services have upgraded to CDAnet version 4 claims. The upgrade requires dental offices to update National Life’s carrier record in the office practice management software. Also included are some carrier claim detail changes.
Effective January 17, 2024 - National Life of Canada Carrier ID. 000021
CDAnet version – change from 2 to 4
Age limit days – change from 10 to 365
Multipart Predeterminations – change to Y (supported)
Request for Outstanding Transaction (04) – change from Y (supported) to N (not supported)
Outstanding Transaction Response (14) – change from Y (supported) to N (not supported)
Claims Processor help desk - 1-877-422-6487
Double check the Public Service benefit plan and certificate numbers to prevent claim assessment delays
August 4, 2023
Canada Life is the administrator of the Public Service Dental Care Plan (PSDCP) and, as of July 1, 2023, the Public Service Health Care Plan (PSHCP). The PSDCP and the PSHCP have different plan numbers and certificate numbers, making it important to use the correct plan information.
Dental claims submitted to Canada Life for reimbursement under the PSDCP must be submitted with the following plan information:
|
The patient’s plan number should match one of these: |
The patient’s certificate number will usually (but not always) be alphanumeric. |
|---|---|
|
Examples:
|
There will be a delay in claim adjudication if dental claims are submitted with the health care plan and certificate numbers.
The only dental claims that can be submitted under the PSHCP are dental accident claims and some oral surgery claims only, once all dental plan payments are exhausted.
Thank you for your help in ensuring that dental claims for the PSDCP are submitted with the correct plan information so that they can be adjudicated as quickly as possible.
Note: Sun Life is the current administrator of the Pensioners’ Dental Services Plan (PDSP). All dental claims must continue to be submitted to Sun Life for patients covered under the PDSP.
CDA Secure Send Mobile App
November 17, 2022
CDA Secure Send mobile app is available to download free from the IOS & Android app stores. With only a few taps on your office device, dentists and the dental teams can send CDA Secure Send messages, send and receive referrals and patient information securely. For more information, visit the CDA Secure Send app webpage
Beneva accepts CDAnet file attachments
November 17, 2022
Effective November 10, 2022, Beneva started accepting CDAnet file attachments (patients records) for claims and predeterminations submitted electronically.
Please ensure you update the carrier record in your software to enable the attachment transaction:
- Attachment (09)
- Attachment Response (19)
The attachment option allows offices to send patient records such as x-rays, images or other documents along with the patient’s claim or predetermination. This claim feature reduces processing times as well as postage and administrative fees associated with the mailing of documents. When sending attachments to these carriers you must indicate on the initial claim or predetermination that an attachment also known as “materials will be forwarded” will be sent.
If you are unsure how to make the setting changes, please contact your software vendor.
Read Beneva’s full communication.
REMINDER - AGA Financial Group Inc. Carrier ID 610226
November 17, 2022
As a reminder, AGA Financial Group Inc/Group Financier, AGA. is a CDAnet claims processor using the carrier ID 610226. They are a claims processor for multiple third-party administrators (TPAs) and their plan member cards include the TPA name and logo with AGA Financial Group carrier ID 610226.
AGA Financial Group Inc. is likely listed as Group Financier, AGA in your practice management software. To improve your search for their carrier record in your software, we recommend you update the carrier name to AGA Financial Group Inc./Group Financier. If this is not an option in your software, please contact your software vendor.
Regardless of the listed carrier name, claims submitted with the carrier ID 610226 will be successfully routed to AGA Financial Group Inc./Group Financier, AGA.
Read the full notice and view the sample card.
REMINDER - MDM Insurance (Carrier ID 601052) updated supported transactions
November 17, 2022
Please ensure your practice management software has the updated information for MDM Insurance along with the additional claim transactions they are now accepting:
- CDAnet Version: 4
- Age Limit (days): 365
- COB Claim (07)
- Predetermination EOB (23)
Depending on your practice management software, you may need to make some setting changes for MDM Insurance. If you are unsure how to make the setting changes, please contact your software vendor.
For a full list of MDM Insurance supported transactions please visit the CDAnet Carrier page
REMINDER - Check GroupHEALTH Benefits Solutions (myGroupHealth) address
November 17, 2022
GroupHEALTH Benefits Solutions (myGroupHealth) would like to ensure you have their correct claims processing mailing address on file and to make sure claims are sent to the below address and not their head office.
myGroupHEALTH Claims
626-21 Four Seasons Place
Etobicoke, ON M9B 0A6
More insurance carriers accept CDAnet file attachments
October 26, 2022
Effective September 18, 2022, the following carriers started accepting CDAnet file attachments (patient records) for claims and predeterminations submitted electronically:
- Desjardins Insurance (carrier ID 000051)
- Groupe Financier AGA Inc. (carrier ID 610226)
- UV Insurance (carrier ID 610643)
Please ensure you update the carrier records in your software to enable the attachment transaction:
- Attachment (09)
- Attachment Response (19)
The attachment option allows offices to send patient records such as x-rays, images or other documents along with the patient’s claim or predetermination. This claim feature reduces processing times as well as postage and administrative fees associated with the mailing of documents. When sending attachments to these carriers you must indicate on the initial claim or predetermination that an attachment also known as “materials will be forwarded” will be sent.
If you are unsure how to make the setting changes, please contact your software vendor.
Read Desjardins insurance full communication.
Read Group Financier’s full communication.
Read UV Insurance’s full communication
New Carrier! HPEI – Public Health Dental Programs - Carrier ID 000130
September 16, 2022
Effective September 26, 2022, HPEI – Public Health Dental Programs will start accepting CDAnet dental benefit claims with Carrier ID 000130. Please ensure you add their carrier information to your software. If adding a carrier is not an option, please contact your software company to ensure HPEI – Public Health Dental Programs is set-up for your patient’s next visit.
Practice Management Software Setup Information
- Carrier Name: HPEI-Public Health Dental Programs
- BIN/Carrier ID: 000130
- Network: instream
- CDAnet Message Version: 4
- Age limit: 90 Days
Supported CDAnet Transactions:
- Claim (01)
- Claim Acknowledgment (11)
- Claims Explanation of Benefits (21)
Access more information on the HPEI Public Health Dental programs.
Why using the correct UIN (Unique Identifier Number) on insurance claims is important
March 31, 2022
Dental benefits play an important role in contributing to patients visiting their dentist for oral health services. CDAnet was developed as an important value-added service for managing dental benefit claims. It provides nearly 90% of licensed dentists across Canada with the ability to assist patients with claiming dental benefits in an efficient and secure manner.
In Canada, our current dental benefit claim ecosystem has no contractual obligations between dentists and insurance carriers. However, it is important to closely follow the principles from the CDAnet/ITRANS subscription agreement. To help keep your practice running smoothly, here are important reminders when assisting patients with claiming dental benefits.
Never combine claims by more than one dentist under a single UIN:
Insurance carriers use the information contained in the claims they receive to establish profiles of the dentists identified in these claims. Grouping claims for work performed by more than one dentist under the UIN of just one dentist may appear to ease the administrative burden at your office; however, it distorts the profile of the dentist whose UIN appears on the claims in a way that could attract unwanted attention from insurance companies.
Serious implications of using wrong UIN on claims:
Misrepresenting the UIN of the providing dentist when using CDAnet to transmit patients’ claims is serious. Key principles of the CDAnet/ITRANS subscription agreement states:
|
3.4 (f) You warrant that the electronic submission of any Dental Benefit Claim by You or any of your End Users constitutes a certification that the Claim contains an accurate and complete statement of:
|
Inaccurate representation of any of the above principals could lead to the accusation of fraud and/or being subject to administrative penalties as severe being excluded from the approved provider list of one or more insurance companies.
Not registered for electronic claims? What you can do now:
Associate dentists can be easily set up to send CDAnet electronic claims in a matter of minutes. Here are two fast and easy options:
- The office can sign in to the CDA Practice Support Services (PSS) website and send an invite to the associate dentist to join the office; or
- The associate dentist sign in to the PSS website and request to join the office.
Need Assistance?
For more information, please read this FAQ on subscribing to CDAnet/ITRANS. If you have questions, please email CDA at pss@cda-adc.ca or call 1-866-788-1212, Monday to Friday, from 7:30 a.m. to 8:00 p.m. EST.
La Capitale is rebranding to Beneva
January 17, 2022
As of January 17, 2022, claims submitted to La Capitale (carrier ID 600502) will be adjudicated under the insurer name La Capitale/Beneva.
What you need to know:
- As part of the transition process, their members will continue to use their La Capitale card until they receive their new Beneva card.
- Claims should continue to be submitted with the CDAnet carrier ID 600502. To avoid confusion with processing CDAnet claims, in your practice management software update the insurer name for carrier ID 600502 to La Capitale/Beneva. This will make it easier to identify the carrier when patients present the Beneva benefit card.
- Offices can search the CDA carrier list under La Capitale/Beneva or Beneva. Both carrier records will include the carrier ID 600502 with the same claim processing details.
Any question, please contact TELUS Health at 1-866-272-2204.
Read the full notice here.
Reminder to check RWAM Insurance phone numbers
January 17, 2022
RWAM (carrier ID 610616) would like to ensure that your contact records for them include the below phone listings. Their old phone listing has been reassigned and its been reported to RWAM that dental calls are still being received at their old phone listings.
Toll Free: 1-877-888-7926
Local: (519) 669-1632
The PBAS Group accepts CDAnet e-claims for additional plans
December 9, 2021
Effective January 1, 2022, The PBAS Group (carrier ID 610256) will be accepting Plan 250 – Ontario Dental Plan and Plan 810 – Calgary District Pipe Trades. When sending CDAnet e-claims for patients with these plans, ensure the following carrier information is applied:
The PBAS Group
Carrier Code: 610256
Version: 4
Read the full notice and view a list of plans currently accepting CDAnet e-claims.
COUGHLIN (carrier ID 610105) – switching to TELUS AdjudiCare (000034)
November 9, 2021
On November 1, 2021, Coughlin & Associates (carrier ID 610105) started processing a portion of their plan member claims with TELUS AdjudiCare. Coughlin plan members will receive new benefit cards with new group and certificate numbers including TELUS AdjudiCare, carrier ID “000034”, listed on the back of the card.
Please ensure you verify the patients benefit card to identify if the carrier information should be updated in your practice management software for CDAnet e-claims. If the information is not updated, the patients claim will fail and the office will receive an acknowledgement with an error and a display message to request an update to the patients benefit information.
TELUS AdjudiCare is a claims processor that provides claim processing services for many third-party administrators (TPA’s), using the carrier ID 000034.
If you have any questions, you can contact the TELUS Dental Technical Helpdesk at 1-866-272-2204.
Read the full notice and view the sample card.
November 9, 2021
Canada Life is extending claims age limit up to 90 days
Beginning November 16, 2021, Canada Life will extend their claims age limit from 31 days to 90 days.
To have this flexibility you will need to make an update to the age limit in your practice management software for Canada Life (previously Great West Life) carrier ID 000011. While you make this change ensure that you verify the Canada Life’s claim processing details are set to the following:
Age limit – 90 days
CDAnet version – 4
Coordination of Benefits (07) – yes/enabled
Attachments (09) –yes/enabled
The extended age limit will provide more flexibility, however it’s expected that all patient claims will be transmitted on the date of service. In certain situations dental offices will be able to submit their patient claims up to 90 days from the date of service. Claims older than 90 days cannot be sent with CDAnet and ITRANS.
Alberta Blue Cross migration to TELUS network
October 14, 2021
Starting Jan 1st, 2022, Alberta Blue Cross will no longer accept CDAnet claims through their Alberta Blue Cross/Claimstream network.
It is important that the settings for Alberta Blue Cross (Carrier ID 000090) is configured in your office software to use the TELUS Group B network prior to Dec 31st, 2021.
In June 2021, Alberta Blue Cross began accepting dental electronic claims from the TELUS dental network (Group B). With this change now in place, Alberta Blue Cross will no longer accept e-claims directly through their network after Dec 31st, 2021. ALL dental electronic claims to Alberta Blue Cross must be submitted through the TELUS dental network.
If you need assistance making this change to your software, please contact your vendor for assistance.
REMINDER – TELUS AdjudiCare Carrier ID 000034
August 26, 2021
As a reminder, TELUS AdjudiCare is a CDAnet claims processor using the carrier ID 000034. They are a claims processor for multiple third-party administrators (TPAs). Plan member benefit cards will have carrier ID “000034” and the name “TELUS AdjudiCare” in small print. TPA names/logos will also appear on the cards but can be ignored. If TELUS AdjudiCare is not listed in your practice management software, you will need to add them as a new carrier. If this option is not available in your software, please contact your software vendor.
In the interim, if you have carrier ID. 000034 set up in your system regardless of the name associated with this carrier ID, you can submit claims which will be successfully routed to the correct AdjudiCare TPA via the TELUS Dental Network (Group B).
If you have any questions, you can contact the TELUS Dental Technical Helpdesk at 1-866-272-2204.
Read the full notice and view the sample card.
Industrial Alliance Groupe Financier does not support CDAnet Claim Reversals
August 26, 2021
Industrial Alliance Group Financier (IA) carrier ID. 000060 currently does not support CDAnet claim reversals. This means that claim reversals cannot be processed electronically through your practice management software. Until further notice, dentists and office staff can call IA at 1-877-422-6487 and request a claim reversal. All claim reversal requests must be completed the same day as the claim submission. Their agents will ensure prompt processing of these requests.
To update your software, change the configuration settings for carrier ID. 000060, and disable the following transactions
- Claim Reversal (02)
- Claim Reversal Response (12)
Changes to Desjardins Insurance’s (Insurer No. 000051) adjudication service
July 19, 2021
As of January 1, 2021, Desjardins Insurance changed their claim processor from Express Scripts to TELUS Assure. On August 23, 2021, they will transition their final groups. With this milestone date, Desjardins Insurance will begin to offer new CDAnet claim process options!
Click here to read the full notice.
Empire Life Insurance updated supported transactions
August 17, 2021
Effective June 17th, 2021, Empire Life Insurance started accepting additional claim transactions:
- Claim Reversal (02)
- Claim Reversal Response (12)
- PreDetermination EOB (23)
- Claim EOB (21)
Depending on your practice management software, you may need to make some setting changes for Empire Life. If you are unsure how to make the setting changes, please contact your software vendor.
For a full list of Empire Life Insurance supported transactions please visit the CDAnet Carrier page.
New Carrier! BG Benefit Administrators - Carrier ID 000128
March 18, 2021
Effective March 1st, 2021 Bilsland Griffith Benefits Administrators (BG Benefits Administrators) started accepting CDAnet Dental benefit claims with Carrier ID 000128. Please ensure you add their carrier information to your software. If adding a carrier is not an option, please contact your software company to ensure BG Benefits is set-up for your patients next visit.
Manion, GroupHEALTH & Group Source start accepting Coordination of benefits (COB) electronically
March 15, 2021
As of Thursday, March 18, 2021, offices can send CDAnet COB claims for Manion, GroupHEALTH and Group Source with their office practice management software (PMS). To make this claim option available, offices will need to update their PMS settings for each claims processor. First verify that the CDAnet version is set to "version 4" and enable the "COB 07" claim transaction. Using the CDAnet claims processor list, you can look up a complete list of claim processor details, including additional COB claim processing instructions.
Read the full article here.
Changes to Desjardins Insurance Claim Processing
December 11, 2020
As of January 1, 2021, Desjardins Insurance will begin to transition their claim processing from Express Scripts to TELUS Health service. Continue to submit claims to Desjardins Insurance with carrier ID. 000051.
Click here to read the full statement.
Canada Life accepts file attachments
October 21, 2020
Effective Saturday, October 24th, 2020, Canada Life will accept file attachments (patient records) for claims and predetermination submitted electronically.
Click here to read the Canada Life's full communication.
Great-West Life Joins The Canada Life Assurance Company
January 8, 2019
Effective January 1 2020, Great-West Life, London Life and Canada Life have joined together as The Canada Life Assurance Company.
Click here to learn more.
Accerta Is Changing Network Providers
June 10, 2019
On June 16, 2019, Accerta will change their network provider from instream to TELUS.
Click here to learn more.
Check your ITRANS ICA software version —you may not be able to send CDAnet e-claims
April 30, 2019
Effective July 1, 2019, offices using Windows computers (not Mac users) will need to ensure their ITRANS Communication Application (ICA) software has been updated to version 3 or newer. The current version is 4.1. Mac users will not be affected by this software change.
Click here to learn more.
TELUS AjudiCare - New Carrier ID 000034
December 13, 2018
Effective January 1st, 2019, TELUS AdjudiCare (previously known as Symbility or AUTOBEN) will begin to use the carrier ID 000034 to process claims for their clients.
Click here to learn more.
Great-West Life is upgrading to CDAnet version 4
November 26, 2018
On Nov. 30, 2018, Great-West Life will upgrade their dental claims system and process claims with CDAnet version 4. Two important benefits of this upgrade are:
- Predeterminations will be processed immediately when possible.
- Coordination of Benefits will be accepted. This means when Great-West Life is the secondary claims processor you can send the secondary benefit claim right away.
Click here to learn more.
ESORSE will no longer be accepted on the TELUS Group B network
November 23, 2018
Effective November 25, 2018, ESORSE (carrier ID 610650) will no longer be accepted on the TELUS Group B network. This means you cannot send e-claims to ESORSE and will need to complete a paper dental claim form.
Pacific Blue Cross Accepts Coordination of Benefits! CDAnet 07 Transaction
Save time and mailing expenses by sending your Coordination of Benefits (COB) claims electronically to Pacific Blue Cross (PBC).Alberta Blue Cross now accepts patient records with CDA Secure Send
When your office submits a claim or predetermination and diagnostic records are required, you can now use CDA Secure Send to securely submit your patient records electronically to Alberta Blue Cross (ABC).
GroupHEALTH has two Carrier IDs
Verify the carrier ID number on the patient’s benefit card to avoid inaccurate claim submissions.Equitable Life of Canada is moving to real-time claim processing and CDAnet version 4
On July 21 2018, Equitable Life of Canada will be upgrading their systems to begin processing claims in real-time using CDAnet version 4. This means you will receive an immediate response for predeterminations, claims and reversals.Equitable Life claim system will be temporarily unavailable for claim processing on Saturday, July 21, 2018 and will resume on Monday, July 23, 2018.
GroupSource has a new Carrier ID.
Effective August 1, 2018, some GroupSource clients will be covered under a new Carrier ID. 605064. This change only applies to some of clients; others will remain on the existing Carrier ID. 610099.
Sun Life new monthly dental cheque payments
Starting August 2018, Sun Life Financial will begin issuing dental cheques and claim statements monthly. For daily payments, Sun Life offers Electronic Funds Transfer services.
GroupHEALTH New Carrier ID. 000125
GroupHEALTH would like to remind you that in November, 2017, they started using a new Carrier ID (000125) for a portion of their clients. This change only applies to some clients; others will remain on the existing Carrier ID., 610099.
Mandatory Consent
As we continue to move to a paperless environment, we would like to remind offices that its mandatory to obtain the patient’s consent to send their personal information to insurance companies. The signed consent form should be maintained as a record in the patient’s file.
Johnson Inc. conversion to Express Scripts
Johnson Inc. will convert their dental plans to Express Scripts Canada. All electronics claims should continue to be submitted to carrier ID. 627265.
Is it time to renew your CDA Digital ID?
The CDA Digital ID.’s are used by ITRANS Claims Service to authenticate dentists when sending e-claims or CDA Secure Send messages. The CDA Digital ID.’s was issued for a 3 year period and most dentists will be required to renew them in 2018.
RBC Insurance - Address Information to send a Claim Form
September 13, 2017
Please note, when you send your claim form to RBC Insurance via Canada Post, please use the following address:
RBC Insurance Company
Attention: Dental Department
PO Box 1614
Windsor, Ontario N9A 0B9
Change to the dentist payment process - Industrial Alliance Financial Group
June 29, 2017
Transactions relating to assigned benefit payments to dentists sent to iA Financial Group will be paid by instream DIRECT PAY, a national provider specializing in secure online services for the dental community and insurers. This new process will be effective on June 30, 2017. There is no change to the electronic claims or dentist assignment processes. Download the PDF file for more information.











