Frequently Asked Questions
Listed below are answers to some frequently asked questions about CDAnet and ITRANS. If you need more information, please contact us at 1-866-788-1212 Monday – Friday from 7:30 AM to 8:00 PM Eastern Standard Time
CDAnet Resources
The CDAnet Dental Office User Guide provides information on CDAnet e-claim transactions and carrier responses. This material is recommended for staff processing claims.
The CDA maintains a list of carriers available on our website. You can look up claim processing details for each carrier, including their CDAnet version, list of supported claim transactions, COB processing details and network information. To ensure you are getting the most out of your office claim processing, use this information to keep the carrier information up to date in your practice’s software.
CDAnet/ITRANS Support
Dentists can subscribe to the CDAnet & ITRANS service when licensed and a member in good standing with the provincial/territorial dental association, or with CDA as an Affiliate Member in Quebec. A dentist must be a member of the provincial dental association (or a CDA Affiliate Member in Quebec) in each of the provinces or territories they wish to use CDA Services such as CDAnet, the ITRANS Claims Service and CDA Secure Send.
There are two options. The first option involves the dentist or office staff signing into the CDA Practice Support Service (PSS) website and sending an invite request to the new dentist to add them to the CDAnet office account. The dentist will receive an email notification to approve the invite request, and to subscribe to CDAnet and ITRANS services
The second option requires the dentist to sign into their PSS account and to select the “Request to join an office” option. For this, the dentist will need the CDAnet office ID. The process will include subscribing to CDAnet and ITRANS before the request is sent to the office. The office will receive an email notification to approve the request.
For both options, the insurance carriers will receive the request to add the new dentist in the next update file that the CDA sends bi-weekly.
Sign in to the CDA Practice Support Services website. From the subscriptions tab, select the CDAnet office ID, and complete the subscription agreement process. The subscription process is required for each dental office that a dentist practices in. The insurance carriers will receive the dentist record in the next CDA bi-weekly update file and the dentist will be added to their system for authorized claim submissions.
Dentist or staff with access should sign-in to the CDA Practice Support Services website, and select the CDA Digital ID tab to get a CDA Digital ID secure code.
To install the CDA Digital ID, you will need to know if the office software installs on a server, or if it needs to be installed at every workstation. If you are uncertain, you can verify this information with your software vendor or the CDA help desk can assist you at toll-free 1-866-788-1212. You can reference the CDA Digital ID resource page for more information.
Log in to your PSS account, click "ITRANS Claims", and select "View Details" on any transaction. Under the “General” section, the “O/S” field will indicate ITRANS 1, or if you are using ITRANS 2, it will display your “Microsoft Windows or Linux Operating System version”
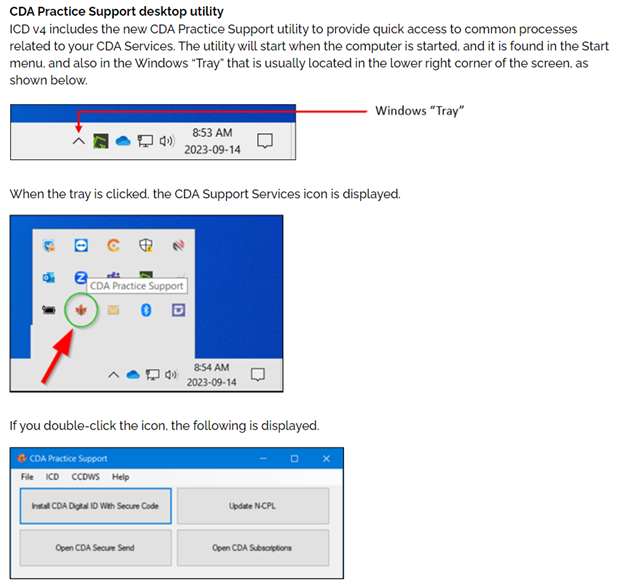
The CDA Practice Support application will start when the computer is started. You can find it in Start menu and in the Windows tray, which is located in the bottom-right corner of the taskbar next to the clock.
The Unique Identifier Number (UIN), sometimes also referred to as a provider number, is a unique number that the CDA assigns dentists once they are entered into the system. The alpha-numeric ID is used to uniquely identify dentist for the submission of patient claims. The UIN is specific to a province and a dentist license type (specialty). Dentists who are licensed in two provinces will have two UIN’s. Also, if the dentist becomes a recognized specialist, the dentist will need to request a UIN update to reflect the license change.
When a dentist’s license number has changed, the dentist’s Unique Identification Number (UIN) must also be updated with the CDA and insurance carriers.
Sign into your account on the PSS website, select the “my info” tab, choose professional information and request your change. CDA will complete the update to your information and the change in UIN will apply to all the CDAnet offices you are in within the same province. You do not need to contact the insurance carriers; they will receive the updated information in the files that CDA sends bi-weekly.
The office ID is a unique number assigned to dental practices when a new office is created in CDA’s system The office ID included in the top right-hand corner of the Explanation of Benefits and Claim Acknowledgement claim response.
You can access the office ID from a dentist’s PSS website account and authorized staff users can view these office ID.’s for each practice the dentist sends CDAnet claims from.
Never. Claims must always be sent under the Unique Identification Number (UIN) of the treating dentist. In cases where the practicing dentist is not registered for electronic claims in the office, send them an invite to get them set-up. If the claim reimbursement should be sent to the dentist practice owner, contact the insurance carrier and make arrangements to route the payment. However, do not process a claim under a dentist’s UIN that has not provided the services.
The dentist/staff will need to contact each carrier and determine what options and process is available. Look-up carrier contact information on the CDA Carrier webpage.
No. An independent dental hygienist must submit benefit claims under their own Unique Identification Number (UIN) as an independent dental hygienist using their own system, not CDAnet. When transmitting dental claims with CDAnet and ITRANS, only the services provided by the treating dentist, or a dental hygienist employed by the dentist, can be transmitted under the dentist’s UIN.
The dentist or authorized office staff can sign-in to the Practice Support Services website, select the office and complete the address update. You do not need to contact the insurance carriers; they will receive the updated information in the files that the CDA sends bi-weekly.
Sign-in to the Practice Support Services website, select the office ID. Go to the office user section, and select the new dentist role to complete the update. This change can only be completed by dentists or office staff that have access.
Yes, an office must obtain the patient’s authorization to send claims electronically on their behalf. The authorization information and suggested disclosure can be found in the CDAnet Dental Office User Guide.
Claims Processing Procedures and Transmission Issues
If the dentist recently subscribed to CDAnet and ITRANS, it’s likely that the insurance carrier has not added the dentist to their system yet. It can take up to 7 business days for each carrier to process the new record. If the office continues to receive this error message or the dentist didn’t recently subscribe, please contact the CDA help desk at toll-free 1-866-788-1212, Monday – Friday from 7:30 a.m. to 8:00 p.m. EST.
First, verify if there is a carrier network issue posted to the ITRANS claim status twitter feed. If it’s not related, contact your practice management software vendor.
First, verify if there is a carrier network issue posted to the ITRANS claim status twitter feed. If it’s not related, contact the CDA Help Desk toll-free at 1-866-788-1212. A technical representative can review the error message and assist the office with resolving the issue.
Generally, the office should receive an error message. If this is not the case, the office should contact the CDA Help Desk toll-free at 1-866-788-1212 and a technical representative can assist you.
Check the claim error message, correct the error(s) and resubmit the claim or predetermination. If you receive an error that you don't understand or the office system does not accept the changes, call the CDA Help Desk at 1-866-788-1212.
It means that the carrier ID number you have programmed in your practice management software is incorrect. Verify the carrier information on the CDA carrier webpage and make any necessary changes. If you're unsure on how to change this information, contact your software vendor for additional help.
Yes, CDAnet claims may be transmitted through ITRANS 24/7, including holidays. If the carrier system is not available, the network will acknowledge receipt of the claim and forward the claim to the carrier system when it becomes available.
No, a claim reversal can only be submitted through the office software on the same day the claim was sent. If it’s not within the same day, contact the insurance carrier for assistance. Be sure to have the Explanation of Benefits or Claim Acknowledgement available when you call.
The claims processor system was unable to handle your request for a claim reversal at the time it was submitted. Try to reverse the claim again later in the day. If you are unable to reverse the claim on the same day, contact the carrier for more information.
The plan member should continue to submit the patient’s claims on paper using the Standard Dental Claim form.
In some cases, software vendors will make updates to your software carrier list. However, the office is generally responsible to ensure that carrier information is updated as changes are made. You can access updated carrier information from our CDAnet carrier list.
To get the most out of your claim processing, it’s important that carrier information is always up to date. If an insurance carrier upgrades from CDAnet version 2 to version 4, and the change is not made in the office software, the office will not be able to take advantage of the additional claim types like coordination of benefits, attachments, and additional lab fee procedure lines.
The CDA will send an email communication to inform offices of any CDAnet carrier changes. A list of carriers and their claim processing details is also available on the CDA website. At any time, you can check the list and get up to date information. In most cases, your dental software vendor will require offices to independently make the carrier updates in the office software. Its important that the carrier claim processing details are updated so that you are getting the most out of your CDAnet e-claim processing.
A carrier must be using CDAnet version 4. Most are, but an office can verify carrier information on the CDA carrier webpage. Once you’ve confirmed the carrier is version 4, check the settings in your software and ensure that the carrier’s CDAnet version is set to 4 and the coordination of benefits 07 transaction is enabled. If you need assistance with this, contact your dental software vendor.











