Bridging the Financial Gap in Dental Care
Building a sustainable and effective federally funded program
Building a sustainable and effective federally funded program
History of Publicly Funded Dental Care in Canada
When Canada’s medicare system was established via the Medical Care Act of 1966, dentistry was not included.18 Around this time, many provinces began to set up publicly-funded dental care initiatives to promote and improve oral health—particularly among children. Although this program, and many others, showed positive results, many were later cancelled or scaled back due to shifting government priorities. Given the ad-hoc nature in which these programs were launched—outside of a broader national approach to health care—oral health became an easy target for cost-cutting initiatives.
Today, in Canada, publicly funded dental care continues to be mostly delivered by private dental clinics, usually owned and operated by dentists. There are major differences between programs in different provinces and territories, including eligibility criteria and what is covered in each jurisdiction. The Canada Health Act covers some surgical-dental services provided by a dentist in a hospital, when a hospital setting is required to properly perform the procedure. Because health care is mostly a provincial and territorial responsibility (with some exceptions), many provinces continue to put most of their health care funds into social assistance programs and public health programs, while leaving public dental programs consistently underfunded.

Community water fluoridation, which began in Canada in the 1940s, is a public health measure that has positively impacted the oral health of millions of Canadians.20 Dentistry has long been an advocate of community water fluoridation because it is a cost-effective, accessible and preventative measure that has been proven to decrease the incidence of cavities.
State of Oral Health in Canada
Although data on the oral health status of Canadians is limited, the most recent comprehensive national survey with clinical data on oral health outcomes was carried out in 2007-08 through the Canadian Health Measures Survey (CHMS). Health Canada published a report on the dental health of Canadians in 2010, based on the results of the CHMS, that showed that 75% of Canadians visited a dental clinic annually and 86% did so at least once every 2 years. The data demonstrated a significant improvement from the Nutrition Canada survey done in the early 1970s, when barely half the population consulted a dentist on an annual basis.21
A key oral health measure for comparative purposes is the decayed, missing and filled teeth (DMFT) index measure. The measure is taken in 12-year-olds. In Canada, the mean DMFT index is 1.02, which is better than most high-income countries where the average mean DMFT is 1.60, according to the most recent data from 2006.22 Canada also ranks favourably in comparison to other high-income countries in prevalence of severe chronic gum disease (less than 10% of the population aged 15 and over) and incidence of oral and lip cancer (2.5-4.9 per 100,000 people).23
Not all data about Canadian oral health is as positive. Several studies have shown that oral health outcomes among Indigenous Peoples are significantly lower than the non-Indigenous population. Other studies show that low-income Canadians are less likely to visit a dentist.24
There are economic costs related to oral disease in Canada. The percentage of Canadians who have experienced time-lost from normal activities for oral health reasons is 39.1%, and over 2 million school days are lost annually due to dental visits or dental sick-days.21 It is estimated that over 4 million working-days for adults are lost annually due to dental visits or dental sick-days.21 There are also other costs associated with emergency department visits for oral disease.
Canada in a Global Context
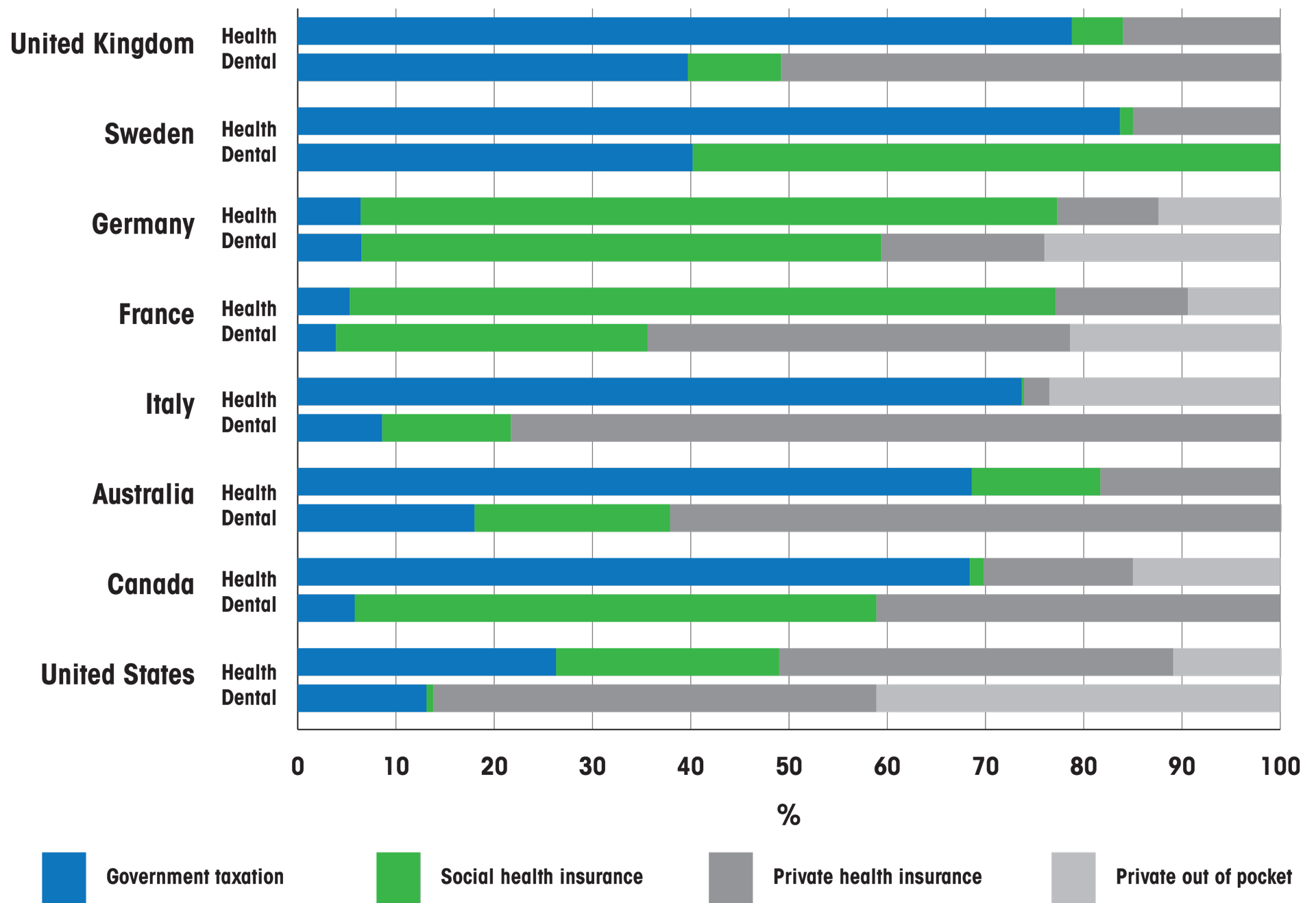
Alternative models of care or funding in other countries could provide some insight into how to alleviate inequities in access to care in Canada, although it is important to note that dental programs in other nations are not standalone and are embedded in each country’s health care system. The organization of oral health care delivery systems and coverage of dental care varies across high-income countries; however, the one common element is access to care barriers. Many dental services require substantial cost-sharing in most countries, leading to high out-of-pocket spending. Socioeconomic status is a main determinant for access to dental care internationally, but other factors such as geography, age and comorbidities can also inhibit access and affect outcomes. Coverage in most oral health systems is targeted at treatment and less at preventative oral health care.
Allin S, Farmer J, Quiñonez C, Peckham A, Marchildon G, Panteli D et al. Do health systems cover the mouth? Comparing dental care coverage for older adults in eight jurisdictions. Health Policy. 2020;124(9):998-1007.
With a 75% annual population utilization rate, Canada is a leader amongst high-income countries in this metric, even compared to countries with higher levels of publicly funded dental care: Australia (48% annual utilization rate), the United States (66% ), the United Kingdom (51%), and France (64%). Although Canada’s annual utilization is relatively high, access to dental care by the most vulnerable groups is a major challenge. Outlined below are some features of the oral health care delivery systems of seven other countries, which are based on a wide range of financing models and strongly influenced by the organization of the health care system.25 26 27 28 29
In Sweden, there are both public and private oral health care providers. The public dental service (PDS) is operated by all 21 county councils/regions. Less than half of dentists work in private practices. Most dentists work in public dental clinics or municipal health centres that have a focus on dental care provision for children and adolescents. Approximately 60% of adult patients visit private dental care providers, while 40% visit the PDS. Dental care is free up to the age of 23 and all others receive an annual general dental care allowance to encourage dental check-ups and preventive care. People with certain illnesses or conditions receive a special dental care subsidy and, in addition, most dental care in Sweden is subject to a high-cost protection scheme, which aims to protect patients from very high dental care costs. Even though private out-of-pocket makes up over 60% of all sources of financing for dental care, only 2% of the population in the country reports unmet dental care needs. Nonetheless, dental care is not included in the basic benefits package, and it is subject to higher co-payments for adults above the age of 24. A recent government report recommended major reform to the dental care system in 2026 to tackle inequalities in access.30 31 32 33
Germany has a statutory health insurance system, predominantly based on social health insurance as a source of financing for over 80% of health care and half of dental care. Almost 90% of Germans belong to not-for-profit “sick funds,” which must provide a legally prescribed package of health care. There is a requirement to get this social insurance, which is based on a cut-off income for employed people. Premiums for membership in these funds are shared between employees and employers. The sick funds are not-for-profit organizations, and membership in a sick fund entitles the member to a package of free basic dental care, with advanced treatment options sometimes requiring significant patient copayments. One of the challenges in Germany is that state funds are decreasing (they are also being amalgamated) so there has been a reduction of services to contain costs. There is also a sizable administrative burden built into the system and delays in treatment; people often wait a year to get care for some conditions. Taking everything into account, it has been reported that Germany’s safety net has resulted in an excessively high cost for Germany’s oral health system, and that the potential for improving both efficacy and efficiency in German dental care persists.34 35 36
Japan has a universal health and dental system, where all providers are a part of the system and charge on a fee-for-service basis. Patients generally pay a 30% copayment for dental care. There are exceptions for those who are not able to afford a copayment. There is also a variation across Japan of oral health indicators, although in general the nation has improved over the last decades. Japan also has a unique and well-designed system to deliver oral health care to its rapidly growing population of seniors, which is beneficial because it has an integrated medical/dental approach.37 38 39
The United Kingdom has a national public dental service that finances over 40% of dental care, however there is a private sector as well that accounts for about half of all financing for dental care. A recent government report found that there are marked inequalities in oral health in England across all stages of life and over different clinical indicators such as dental decay and related quality of life measures. The relative inequalities in the prevalence of cavities in 5-year-old children in England has increased. There are also inequalities in the availability and use of dental care across ages, gender, geographies, and different social groups. As well, a growing number of dentists do little or no publicly funded work, citing problems with the dental contract, and this has led to “dental deserts,” areas with a considerably low level of publicly funded dentists, particularly in rural and coastal areas.40 41
Brazil is the only country in the world with a universal health care system with the aim of guaranteeing delivery of all levels of health care, free of charge, to a population of over 200 million inhabitants by means of a unified health system. As part of this initiative, Brazil implemented a country-wide National Oral Health Policy in 2004, which, in effect, made the delivery of oral health care universal. Recent findings demonstrate that although there was a reduction in the percentage of individuals who had never visited a dental professional, many people still do not have access to dental care. Decreasing cost barriers alone has not resulted in adequate access to dental care and more comprehensive policies for addressing the wider determinants of inequality are needed.42
In the United States, a 2021 National Institutes of Health report reviewed the state of the US oral health care system, achievements made since 2000, and remaining challenges. The percentage of Americans who had an annual oral health care visit increased from 2000 through 2018, particularly among children younger than 18 years of age. Annual visit rates among older adults (over age 65) increased to 66% in 2018, but rates did not change among adults. Differences in access to oral health care exist across race and income for adults older than 18. Access to comprehensive oral health care continues to be one of the biggest challenges within the oral health care system and a key driver of oral health care inequity; many Americans cannot afford the high deductibles and copayments of private dental insurance programs. Public insurance coverage has increased since 2000 but remains limited for many low-income, minority, and older adult populations.43 44
In Australia, the government does not cover the costs of most dental care as it does with other health services. Less than 20% of dental care is financed through the government; 20% is covered through private insurance and more than 60% is paid out-of-pocket by patients. However, medicare does pay for some essential dental care for some children and adults who are eligible. The main aim is to provide dental coverage for children between the age of 2 and 17, and eligibility is income based. Eligible children are provided with up to $1,000 in benefits for basic and preventive dental care. Data shows that 10% of people who saw a dental professional in Australia received public dental care, and 33% who needed to see a dental professional delayed seeing or did not see one, and around 1 in 7 reported that cost was a reason.45