
28
|
Volume 3 Issue 5
S
upporting
Y
our
P
ractice
bitewing radiographs to rule out any new tooth decay
or other conditions. There were no significant findings
upon clinical examination and no causes for concern
were identified.
It is common for patients diagnosed with
schizophrenia to require readmission to hospital
for stabilization as a result of non-compliance with
medication and deterioration of their condition. While
a concurrent history of polysubstance abuse might
have precipitated the patient’s readmission to the
hospital, substance abuse was not an issue at this
particular time in his treatment.
The patient told Dr. Clark he felt “divided in half”
because of his one remaining primary molar. The side
with no primary teeth felt like an adult. The other side,
the one with the retained primary 85, rendered him
feeling like a child or infant. He was having difficulty
dealing with these conflicting feelings, and he
indicated only feeling able to chew on the “adult” side
of his mouth.
Diagnosis
As the investigation did not reveal any significant
clinical findings that could explain the patient’s
discomfort with tooth 85, it was determined that it
was solely a manifestation of the patient’s delusional
thought process.
“Delusions are a common feature of the positive
symptom complex of schizophrenia, meaning that
they are observable while they should not be,” explains
Dr. Clark. “The other two symptom complexes are
disorganized and negative symptoms. This patient
displayed primarily positive symptoms in his overall
diagnosis of the disease, which does carry a better
prognosis with treatment, and often a better response
to antipsychotic medications that are prescribed for
these patients.”
Treatment Plan
“In my experience, retained primary molars in adult
patients can survive quite well for many years, and
there’s no indication that we have to intervene
and extract them. They are an inexpensive way to
retain space and provide some function—while
perhaps limited for this individual,” says Dr. Clark. He
explained this reasoning to the patient. “He was very
pleasant and he listened while we explained the pros
and cons of both tooth retention and extraction,”
Dr. Clark remembers. “I presented him with my
recommendations and explained that I declined to
extract his tooth for the reasons that I had just given
him. While it wasn’t what he wanted to hear, he was
accepting of it.”
The patient returned to the dental clinic to see the
hygienist, and was certainly motivated to look after
his teeth. He was discharged from the hospital shortly
after that time.
a
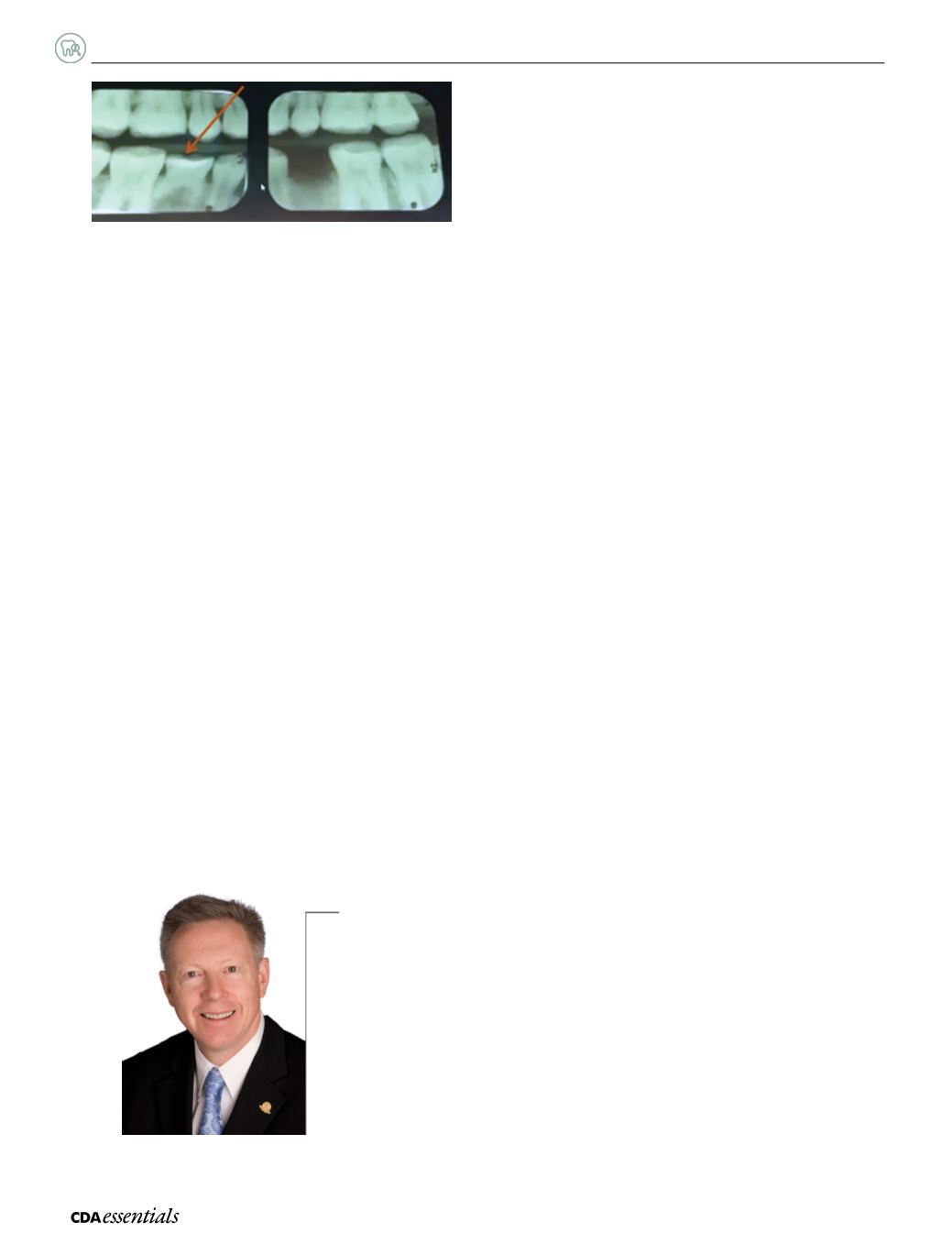
Figure 1:
Bitewing radiographs showing the presence of retained tooth 85,
and the absence of clinical findings explaining the patient’s concerns.
Could extraction have been the solution?
Could tooth extraction have eliminated the delusional thought process? “Sure, we could easily have
extracted the tooth,” recognizes Dr. Clark. “Yet should another practitioner have later recommended
the use of an implant or another prosthetic replacement, there would have been the potential for it to
trigger further delusional thinking or thought processes typical of this positive symptom complex.” For
example, the patient could eventually have perceived the implant as something foreign to him. It could
also have resulted in the delusion of thought broadcasting—another very common delusional thought
process that occurs in patients with this diagnosis—, creating a whole new area of conflict for this
patient. “The simplest approach, and the one I was quite comfortable with, was to decline to remove the
tooth for him at that time,” Dr. Clark concludes.
Dr. David Clark
















