27
Volume 3 Issue 6
|
S
upporting
Y
our
P
ractice
Many drugs and materials commonly used in dental offices
can trigger allergic reactions—antibiotics, analgesics, local anesthetics, resins, etc. It is important to respond
promptly to any suspected anaphylactic reaction as it can develop quickly and potentially be fatal. If you suspect
a patient might be going into anaphylactic shock, consider following the Anaphylaxis Emergency Plan developed
by the Canadian Society of Allergy and Clinical immunology (CSACI)
2
:
➊
➤
Administer epinephrine at the first sign of a known
or suspected anaphylactic reaction.
➋
➤
Call 911 or your local emergency local services.
➌
➤
Administer a second dose of epinephrine after 5 to
15 minutes if the reaction continues or worsens.
❹
➤
Transfer the patient to the nearest hospital (ideally by
ambulance), even if the symptoms are mild or have stopped.
➎
➤
Call the patient’s emergency contact person.
Management of Anaphylactoid
Reactions
Anaphylactoid reactions present with the same clinical
manifestations as anaphylactic reactions, but are not caused by
an immunoglobulin-mediated response. Patients may therefore
experience anaphylactoid reactions without prior sensitization
to an allergen. Anaphylactoid reactions are managed the same
way as anaphylactic reactions.
Following Injection of Epinephrine
It is recommended to raise the legs of a person in anaphylactic
shock to improve blood circulation to the heart. CSACI urges
to avoid “having an individual immediately sit up or stand after
receiving epinephrine as these sudden changes of position may
lower their blood pressure, worsen their condition, and potentially
result in death.”
2
If the patient feels sick or is vomiting, place them
on their side.
The cautionary measure of keeping the patient in a lying position still applies after the emergency medical team
has arrived. “Even if the person is feeling ‘better’, they should
not
stand up or walk themselves to the ambulance,”
stresses Food Allergy Canada (formerly Anaphylaxis Canada) on its website.
3
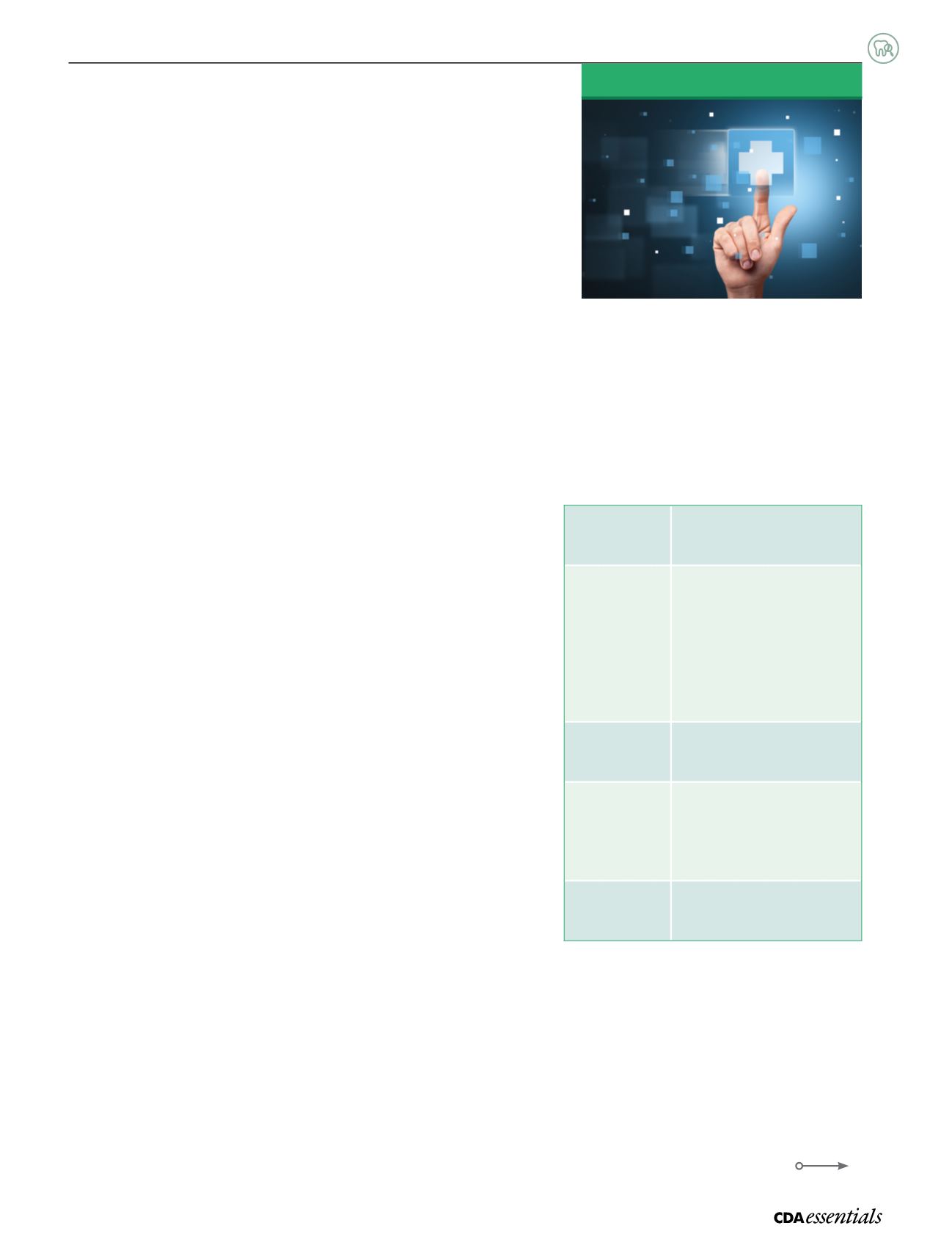
Table 1:
Signs and Symptoms of
Anaphylaxis
Skin system
hives, swelling (face, lips, tongue),
itching, warmth, redness
Respiratory
system
coughing, wheezing, shortness
of breath, chest pain or tightness,
throat tightness, hoarse voice,
nasal congestion or hay fever-like
symptoms (runny, itchy nose and
watery eyes, sneezing), trouble
swallowing
Gastrointestinal
system
nausea, pain or cramps, vomiting,
diarrhea
Cardiovascular
system
paler than normal skin colour/
blue colour, weak pulse, passing
out, dizziness or lightheadedness,
shock
Other
anxiety, sense of doom, headache,
uterine cramps, metallic taste
Source: Canadian Society of Allergy and Clinical Immunology. Anaphylaxis in
Schools & Other Settings. 3rd Edition. 2014.
Managing Medical Emergencies:
Anaphylaxis
According to Health Canada, an estimated 600,000 Canadians may be
affected by life-threatening allergies.
1
Would you know how to recognize
the signs of—and respond to—anaphylaxis should a patient experience
it in your office?
Medical Emergencies